Open Access | Peer-reviewed | Review Article
Birhanu Ayenew*
Nursing department, health Science College, Assosa University, Assosa, P.O box 18, Ethiopia.
Meseret Yitayew
Nursing department, health Science College, Assosa University, Assosa, P.O box 18, Ethiopia.
Digvijay Pandey
Department of Technical Education, IET, Lucknow – 226021, India.
Published: April 18, 2020 DOI: 10.5281/zenodo.3756676
Abstract
The rapid spread of Corona virus disease (COVID-19) across globe coupled with non-availability of treatment has triggered worries worldwide. Among the known measures, regular hand-washing practice among communities and maintaining physical (social) distance according to health care professional recommendations is the best available option to control the spread of COVID-19. Currently, Ethiopia has a very low health care workforce (Medical Doctors, Health Officers, Nurses, and Midwives) density of about 0.96/1000 population, which is 5 times less than the minimum threshold of 4.45 per 1000 population set by the World Health Organization (WHO). Mass use of public transportation, shortage of sanitation material including water, hiding suspected cases, lack of personal protective equipment for health care providers, presence of immune-compromised people are among the major driving factors making Ethiopia one of the challenged developing country in facing this unprecedented COVID-19 spread. In this scenario, this article objective is to analyze the Challenges and opportunities' to tackle COVID-19 spread in Ethiopia, East Africa.
Keywords: Ethiopia, coronavirus, COVID-19, 2019-nCoV, pandemic, public health emergency.
| Citation: Birhanu Ayenew et.al. (2020) Challenges and opportunities to tackle COVID-19 spread in Ethiopia, Journal of PeerScientist 2(2): e1000014. |
| Received: April 11, 2020; Accepted April 16, 2020; Published April 18, 2020. |
| Copyright:© 2020 Birhanu Ayenew et.al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. |
| Data Availability: All relevant data are within the paper and its Supporting Information files. |
| Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. |
| Competing interests: The authors have declared that no competing interests exist. |
| *E-mail: birhanua2015@gmail.com | Phone: + (25) –1947437698. |
Introduction
The 2019 novel corona virus has been named 2019-nCoV and the disease it causes is called corona virus disease 2019 or COVID-19 [1]. 2019-nCoV was first identified in Wuhan, China in late December 2019 [2]. This virus causes contagious respiratory disease and responsible for the ongoing outbreak with pneumonia-like infection in humans [3]. On February 11, 2020, the World Health Organization (WHO) Director-General, Dr. Tedros Adhanom Ghebreyesus, announced that the disease caused by this nCoV is named as "COVID-19," which is the acronym of "corona virus disease 2019” [4]. Due to the increasing number of cases in China and outside China, the WHO declared corona virus as a global health emergency [5]. The number of cases infected by corona virus outside China has increased many folds within a span of few days, claiming thousands of lives across 192 countries population infected with COVID-19 [6], forcing WHO to declare COVID-19 as a pandemic disease [7]. As of April 09, 2020, there are about 74 laboratory-confirmed COVID-19 infected cases reported in Ethiopia, with a steep increase in the number after March 16, 2020 (figure 1).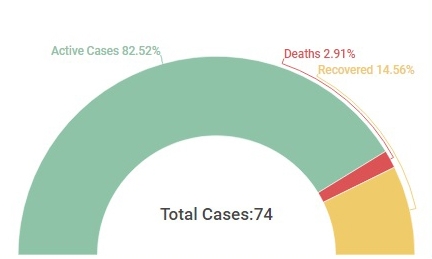

Figure 1: a) Total number of laboratory-confirmed COVID-19 cases, active case, deaths and daily deaths reported in Ethiopia. Figure credits: Worldometers. b) Ethiopia map showing the region in red color with laboratory-confirmed COVID-19 cases identified. Figure credits: Wikipedia.
The corona virus pandemic is causing large-scale loss of life and severe human suffering and public health crisis without precedent in living memory, testing worldwide communities to tackle it [8]. Absence of previous experience in handling 2019-nCoV is part of the reason why it is hard to contain the spread of this particular virus. Since this virus is newly emerged making population highly susceptible and can easily pass from person to person, makes it dangerous [9].
Ethiopia, a developing country from East Africa with a very low health care workforce density of about 0.96 for every 1000 population coupled with shortage of hospitals, mass use of public transportation, shortage of sanitation material including water, hiding suspected cases, lack of personal protective equipment for health care providers, presence of immune-compromised people are among the major driving factors making Ethiopia one of the challenged developing country in facing this unprecedented COVID-19 spread. On the other hand, Ethiopians practice a spiritual and communal life. Warm greetings, handshakes, positive body language (smile or showing a sign of happiness), kissing on the cheek and hugging are part of the normal greetings. Praying together, bowing in front of a priest is commonly practiced. In this scenario, this article aims at analyzing the Challenges and opportunities’ to tackle corona virus (COVID-19) spread in Ethiopia.
The corona virus pandemic is causing large-scale loss of life and severe human suffering and public health crisis without precedent in living memory, testing worldwide communities to tackle it [8]. Absence of previous experience in handling 2019-nCoV is part of the reason why it is hard to contain the spread of this particular virus. Since this virus is newly emerged making population highly susceptible and can easily pass from person to person, makes it dangerous [9]. Ethiopia, a developing country from East Africa with a very low health care workforce density of about 0.96 for every 1000 population coupled with shortage of hospitals, mass use of public transportation, shortage of sanitation material including water, hiding suspected cases, lack of personal protective equipment for health care providers, presence of immune-compromised people are among the major driving factors making Ethiopia one of the challenged developing country in facing this unprecedented COVID-19 spread. On the other hand, Ethiopians practice a spiritual and communal life. Warm greetings, handshakes, positive body language (smile or showing a sign of happiness), kissing on the cheek and hugging is part of the normal greetings. Praying together, bowing in front of a priest is commonly practiced. In this scenario, this article aims at analyzing the Challenges and opportunities’ to tackle corona virus (COVID-19) spread in Ethiopia.
Globalization versus COVID-19
Globalization created dramatic social, political, economic, environmental, and demographic changes. On the other hand, the planet is becoming more and overpopulated [10]. Currently, urbanization has blown up to a point, where more than half of the world’s population is living in cities [11]. These changes are expected to increase the chances to give rise to pandemics and other public health crisis like present COVID-19, especially in developing countries like Ethiopia. Fast and high mobility of people, with increased transportation facilities, international travel and greater inter-connectivity between cities for trade activities within and between cities and countries has became one of the driving factor for rapid spread of COVID-19.
Cultural values and norms of Ethiopia versus COVID-19:
Ethiopians take personal relations seriously and helping each other, even for a total stranger is a common practice. Social occasion or an opportunity to talk about non-work related matters will never be missed for establishing a relationship [12]. Ethiopians enjoy and practice cultures and norms like warm greetings, handshakes, positive body language (smile or showing a sign of happiness) and a show of respect. Kissing and hugging are part of the normal greetings in Ethiopia [13]. Ethiopians live a communal life, i.e. one problem is another’s burden and anything that can alleviate that burden would be appreciated [14]. The spiritual life of the household and community is a foundational aspect of Ethiopian society. Praying together bow in front of the priest is commonly practiced. Cultural values followed by Ethiopians are among high prioritized not-to-do things during pandemic situation like COVID-19 which is contagious in spread.
Lack of medical and healthcare infrastructure in Ethiopia versus COVID-19:
In Ethiopia, Healthcare resources such as the number of physicians, nurses, and midwives are limited. In addition to this, there is a shortage of hospital beds and personal protective equipment. The surge capacity in healthcare systems like the health care workforce, infrastructure, and intensive care capacity is the need of the hour to cope up with COVID-19 pandemic [15]. Ethiopia is one of the countries with a very low health workforce (Medical Doctors, Health Officers, Nurses, and Midwives) density which is 0.96/1000 population [16], which is far below from African health workers density of 2.2/1000 population and 5 times less than the minimum threshold of 4.45 per 1000 population set by the WHO to meet the Sustainable Development Goals (SDG) health targets [17]. Pandemic situation demands more attention and additional essential medical supply such as gloves, masks, syringes, antipyretics, and antimicrobial agents. These supplies are insufficient in developing countries like Ethiopia, even in non-emergency situations.
Homelessness and overpopulation in Ethiopia versus COVID-19
As per WHO Guidelines on Health and Housing, Crowded housing conditions are one among the high risk zone of infections for all the occupants [19]. According to a study conducted in 11 cities of Ethiopia, the number of citizens who live on the streets has reached around 88 thousand. The report also indicates that many of the homeless are found at provincial capitals. Out of the 88 thousand homeless population, children, women, youth and the elderly account for the majority [20]. Section of Ethiopia populations who are homelessness or unsheltered (those sleeping outside or in places which are not appropriate for human habitation) increases the risk of COVID-19 infection spread within the community. Staying home and social distancing are now essential to control the spread of COVID-19 [18].
Expose one, expose us all
According to Ethiopian Demographic Health Survey (EDHS) 2019, the number of persons per sleeping room in Ethiopia is as follows: 38 percent of households have 3 or 4, and 25 percent have only one or two. Households in Rural areas are relatively overcrowded and more risk than urban (figure 2). The mean number of persons per sleeping room in rural areas is 4.3, compared with 3.2 in urban areas. The mean number of the overall crowdedness is 4.1 persons per sleeping room [21]. The increased risk of COVID-19 infection will have an impact on both the residents of crammed dwellings and the rest of the community. Improving the housing conditions of the most marginalized members of our society is an important bio-security measure to contain community transmissions.

Figure 2: This figure shows the proportion of Ethiopian population in urban and rural from 1995 – 2020. Figure credits: Worldometers.
Life expectance of population versus COVID-19
When combined with other factors, such as declining rates of poverty, malnutrition, and other co-morbidities increase the susceptibility and reduce the ease of tolerance. In addition, average life expectancy of Ethiopia is below 60 years compared to global life expectancy which is 67 to 71 years. Since, the prevalence of adult population chances in Ethiopia is low; it may lead to low fatality and increased COVID-19 tolerance capacity [22].
Employee exposure to COVID-19 at work
According to the united state department of labor, employee risks of occupational exposure to COVID-19 during a pandemic may vary from high to very high, medium, or lower (caution) risk. The degree of risk depends upon a part on whether or not job requires close proximity to potentially infected with COVID-19 or whether they are required to have either repeated or extended contact with known or suspected sources of COVID-19 infected among these coworkers, the general public, outpatients, school children or other such individuals or groups.
Very high-risk employees: Healthcare professionals like doctors, nurses, dentists, laboratory personnel collecting or handling specimens.
Medium Risk: Employees who work in overcrowded conditions and comes in frequent contact with general population such as high population density work environments, schools etc., [23].
Low risk: Students who are temporarily canceled their learning activities including kindergarten, pre-school to college and university students and staying home with their families are at low risk and helping to slow the spread.
Transportation system versus COVID-19
In Ethiopia, public transportation is highly vulnerable in boosting outbreaks such COVID-19 pandemic. Heavy focus on hygiene, sanitation, temperature screening at entry sights, and a limited number of the bus seat and onboard cameras to enforce these rules is need of the hour. Social distancing is one of the "non-pharmacologic interventions" that can be used to slow the spread of contagious infections such as COVID-19. This specifically refers to different ways of keeping people separated [24]. Traveling on overcrowded public transportation or mass gathering is absolutely a risk. Public transportation authorities should work to increase the frequency of cleaning buses and trains. Maintaining thorough hygiene and social distancing is an important part of how we can prevent the spread of COVID-19 [18]. Even though, Communicable Disease and Control (CDC) recommends ensuring physical distance in public transportations via accommodating only 50% of its capacity, the Ethiopian public bus transportation system is currently operating at twofold of their capacity. Situations like which can easily boost the spread of COVID-19.
“Infodemic” versus COVID-19
Even though WHO Director-General Dr. Tedros Adhanom Ghebreyesusthe announced that “Fake news spreads faster and more easily than this virus”, and needs attention in tackling this as it is dangerous to the general community” [25]. Over-abundance of information some accurate and truth-worth and some are fake making it dangerous for general public to find trustworthy sources and reliable guidance when they need it the most. In Ethiopia, population generally practice "infodemic" from social media platforms like Facebook, Telegram, Instagram etc., Both government and non-government Ethiopian media should consider implementing the general public rely on use of authorized, up-to-date, truth-worth media as a source of information.
Recommendations
Primarily prevention is more advantageous than secondary and tertiary prevention are the principles of WHO and CDC which is more valuable especially in a developing country. Implementing health care professional recommendations at individual level is invaluable and the only way to tackle COVID-19 spread. Below are few recommendations which we believe world should practice besides Ethiopia, Africa:
- Equity and solidarity: Epidemics are complex events. Complex in their origins, their spread, their effects and reflects their consequences on medical, social, political and economic. So, Equity and solidarity shall be maintained during these periods.
- Use comprehensive outbreak response points:
- Community engagement
- Coordination between responders
- Health information dissemination
- Risk communication_ talk and listen to manage rumors
- Medical and non-medical intervention,
Besides, the following points should be practiced on priority:
- Isolation and treatment (as appropriate) with COVID-19 antiviral medications to all confirmed or potential infected. WHO recommendation of Isolation at home or at healthcare setting; this selection depends upon the severity of illness and /or the capacity of the hospital isolation center and healthcare infrastructure.
- Everyone shall participate voluntarily in informing suspected cases of COVID-19 to nearby healthcare facilities via calls to hotline number 8335 for Ethiopians, for other countries it may vary.
- Closing school teaching learning activity (including public and private schools as well as colleges and universities) and school-based activities and closure of childcare programs, coupled with protecting children and young adults through social distancing not only at school, but also need attention at the community level to achieve reductions of out-of-school social contacts and community mixing.
- Limiting large public gatherings and alteration of workplace environments and schedules to decrease social density and preserve a healthy workplace to the greatest extent possible without disrupting essential services and reduce social distancing measures to contact between adults in the community and workplace.
- Marking standing points, using security to enforce rules and uninterrupted education via use of technological advancements is needed.
- Social media should communicate up-to-date and truth worth information, and rumors should get the fact checked at earliest possible. Remember managing “Infodemic” is as important as managing epidemics.
All such community-based strategies should be used in combination with individual infection control measures, such as hand washing, cough etiquette and social distancing.
Conclusion
Among the known measures to reduce the transmission of COVID-19 regular hand washing practice is the rewarding and physical distance is a major challenge. Presence of a huge number of homelessness people, mass use of public transportation, the maximum size of uneducated people, overcrowding in cities and homes, shortage of sanitation material including water, hiding suspected cases, lack in availability of personal protective equipment for care providers, Presence of immune-compromised people are among the major driving factors make Ethiopia one of the challenged developing country during this pandemic spread. So solidarity and equability with community lead participation are mandatory.
Author’s contribution: BA conceptualized the idea and took care of project administration. BA and MY curated the data, performed formal analysis and Investigation. DP validated, visualized the data. BA, MY and DP wrote the manuscript, edited and finalized. All authors read and approved the final manuscript.
Acknowledgment: Authors would like to thank Walle Kumlachew and Tesfu Zewudu of Health Science college, Assosa University for generously donating their valuable time in providing comments for earlier version of this manuscript.
References
- Zu, Zi Yue, et al. "Coronavirus disease 2019 (COVID-19): a perspective from China." Radiology(2020): 200490.
- Zhu, Na, et al. "A novel coronavirus from patients with pneumonia in China, 2019." New England Journal of Medicine(2020).
- Enitan, Seyi Samson, et al. "The 2019 Novel Coronavirus Outbreak: Current Crises, Controversies and Global Strategies to Prevent a Pandemic." International Journal of Pathogen Research(2020): 1-16.
- Cascella, Marco, et al. "Features, evaluation and treatment coronavirus (COVID-19)." StatPearls [Internet]. StatPearls Publishing, 2020.
- Phelan, Alexandra L., Rebecca Katz, and Lawrence O. Gostin. "The novel coronavirus originating in Wuhan, China: challenges for global health governance." Jama8 (2020): 709-710.
- Basha, Syed Hussain. "Corona virus drugs–a brief overview of past, present and future." Journal of PeerScientist 2.2 (2020): e1000013.
- Organization WH. WHO Director-General's opening remarks at the media briefing on COVID-19-11 March 2020. Geneva, Switzerland. (2020).
- Gostin, Lawrence O. "Pandemic influenza: public health preparedness for the next global health emergency." The Journal of Law, Medicine & Ethics4 (2004): 565-573.
- Schwartz, David A., and Ashley L. Graham. "Potential maternal and infant outcomes from (Wuhan) coronavirus 2019-nCoV infecting pregnant women: Lessons from SARS, MERS, and other human coronavirus infections." Viruses2 (2020): 194.
- Mabuza, Mbuso Precious. "Globalisation, Climate Change, and Disasters." Evaluating International Public Health Issues. Springer, Singapore, 2020. 265-313.
- Jasrai, Yogesh T. "Unit-13 Urban Areas." IGNOU, 2020.
- Lewis, I. M. "The peoples and cultures of Ethiopia." Proceedings of the Royal Society of London. Series B. Biological Sciences1114 (1976): 7-16.
- Prasad, R. Durga. "The Impact of Workforce Diversity on Organizational Effectiveness:(A Study of Selected Banks in Tigray Region of Ethiopia)." (2017).
- Geiger, Martha, et al. "Understanding the Attitudes of Communities to the Social, Economic, and Cultural Importance of Working Donkeys in Rural, Peri-urban, and Urban Areas of Ethiopia." Frontiers in Veterinary Science7 (2020): 60.
- Bauchner, Howard, Phil B. Fontanarosa, and Edward H. Livingston. "Conserving Supply of personal protective equipment—a call for ideas." JAMA(2020).
- Ababa, Addis. "Federal democratic republic of Ethiopia ministry of health." Ethiopia: Postnatal Care(2003).
- World Health Organization. "Health workforce requirements for universal health coverage and the Sustainable Development Goals.(Human Resources for Health Observer, 17)." (2016).
- Tsai, Jack, and Michal Wilson. "COVID-19: a potential public health problem for homeless populations." The Lancet Public Health4 (2020): e186-e187.
- World Health Organization. "WHO housing and health guidelines." (2018).
- Tamire, Elleni. The Livelihood Status of Homeless People: In Addis Ketema, Arada and Kirkos Subcities of Addis. Diss. Addis Ababa University, (2019).
- Ethiopian Public Health Institute (EPHI)[Ethiopia] and ICF. "Ethiopia Mini Demographic and Health Survey 2019: Key Indicators." (2019).
- Jembere, Gizachew Balew, Youngtae Cho, and Myunggu Jung. "Decomposition of Ethiopian life expectancy by age and cause of mortality; 1990-2015." PloS one10 (2018).
- Occupational Safety and Health Administration, U.S. Department of Labor. Guidance on Preparing Workplaces for COVID-19. OSHA 390-03R, (2020):1-32.
- Ryalino, Christopher. "Covid-19: What we know so far." Bali Journal of Anesthesiology1 (2020): 1.
- Zarocostas, John. "How to fight an infodemic." The Lancet10225 (2020): 676.